Preliminary Risk Assessment (PRA)
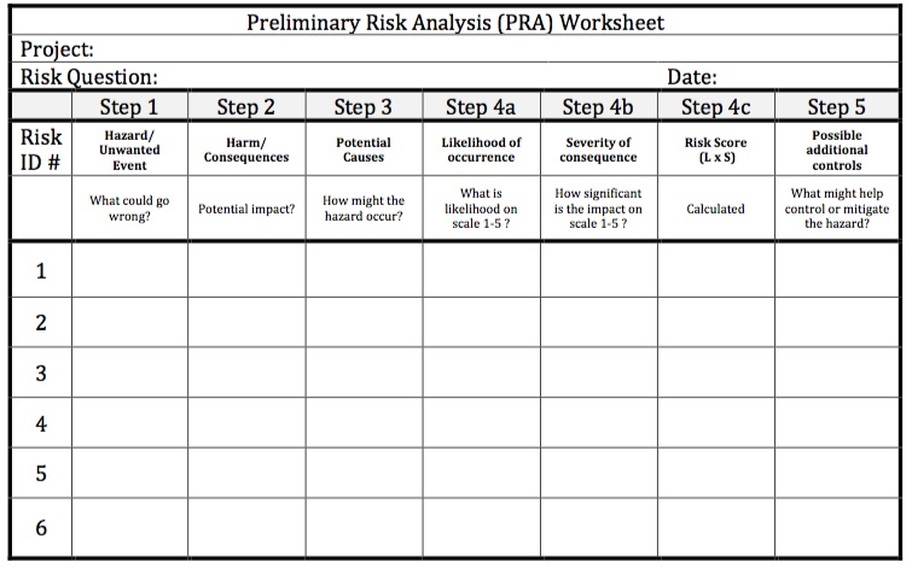
The PRA tool is a first line tool (hence the name “preliminary”) that you would use to determine at a glance the
effects of identified risks. It is often considered as a scaled down version of a FMEA (failure modes and effects analysis) that may be very beneficial in our “hospital risk-based thinking”. One application that might provide immediate assistance to your hospital is with your contracted services. How will you rate the product or service provided by your contracted services to determine the “type and extent of control” necessary for your
contracted services? Below the PRA worksheet, you will find simple instructions on how to use this risk tool that you can use to get you on your way to effective risk management or risk-based thinking.
effects of identified risks. It is often considered as a scaled down version of a FMEA (failure modes and effects analysis) that may be very beneficial in our “hospital risk-based thinking”. One application that might provide immediate assistance to your hospital is with your contracted services. How will you rate the product or service provided by your contracted services to determine the “type and extent of control” necessary for your
contracted services? Below the PRA worksheet, you will find simple instructions on how to use this risk tool that you can use to get you on your way to effective risk management or risk-based thinking.
Here is a brief description on how to effectively use the PRA.
Step 1- Using a cross-functional team, brainstorm “things that could go wrong”. If necessary, you can process all of these potential things that go wrong through the PRA process. You may decide to only manage the Top 5 or 10 depending on how the PRA results look. List these items in column under “Step 1”.
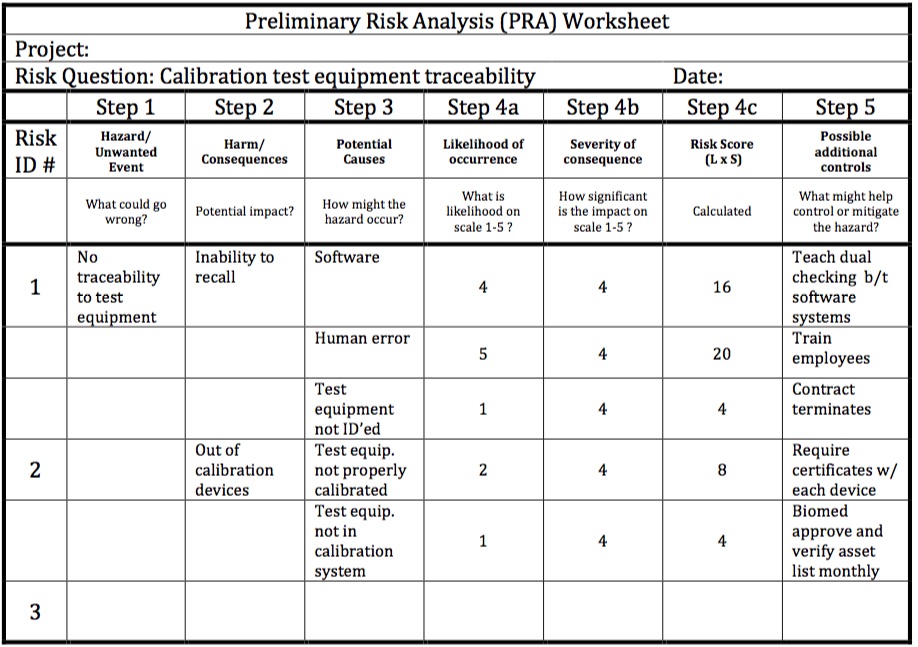
Step 2- Determine the potential impact for each of the items in the first column. You might have multiple impacts for one thing gone wrong. See the sample below how this may look in your PRA.
Step 3- Determine the potential causes for each “thing gone wrong”. There may be multiple potential causes. See the sample below for insights on how this may look in your PRA.
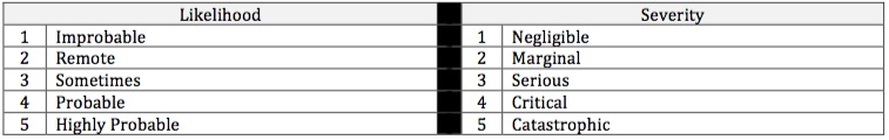
Step 4a- Using Table 2 above, use your cross-functional team to assign a quantitative value to the likelihood of this event occurring.
Step 4b- Using the Table 2 above, use your cross-functional team to assign a value for the severity of the consequence if this event were to occur.
Step 4c- Simply multiply your Likelihood and your Severity columns to create a Risk Score.
Step 5- Consider what possible additional controls could be effectively implemented to mitigate or control the risk.
Additional Notes:
Depending on your risk appetite, you may determine that the identified risk is acceptable in its current state, or you may choose to act on the risk. Hospitals will typically create their own scale for what level is acceptable and what level requires actions (Step 5).
Any Severity of 4 or 5 would usually require additional actions, with few exceptions. Many hospitals are shying away from creating a threshold, such as creating additional actions only for risk scores over 20. Historically, this lends to bias. The result is that many risks are scored less than 20 so as to avoid additional work.
Common rules of thumb for the PRA:
Determine your hospitals risk appetite based on the activity being analyzed.
Assemble the proper cross-functional team to assist in the PRA process.
Employ the usual ground rules for brainstorming in Step 1. If this step is wrong, everything else follows.
Assign as many potential impacts and potential causes as you see fit.
Determine your trigger for action, based on a high severity or a high Risk Score.
If you get stuck on a particular “thing gone wrong” analysis, maybe you need a different tool, such as the FMEA or Fishbone Diagram.
Show value in this process and find ways to link these activities of risk-based thinking to your cost of quality.
Summary:
Getting started with hospital risk-based thinking is easier than you think. You are already doing risk-based thinking, you just need easy access to meaningful tools to assist. The PRA is an entry-level tool for risk assessment. The PRA may be the only tool that you need for assessing risk at your hospital or you may need a more robust tool. Some hospitals will use the PRA as a screening tool to determine if a deeper dive for assessing risk is needed. The purpose of the PRA is to assist hospitals in managing risk. Managing hospital risk appropriately will help create a safer patient environment and allow all healthcare providers to keep their oath of “doing no harm”.
Step 1- Using a cross-functional team, brainstorm “things that could go wrong”. If necessary, you can process all of these potential things that go wrong through the PRA process. You may decide to only manage the Top 5 or 10 depending on how the PRA results look. List these items in column under “Step 1”.
Step 2- Determine the potential impact for each of the items in the first column. You might have multiple impacts for one thing gone wrong. See the sample below how this may look in your PRA.
Step 3- Determine the potential causes for each “thing gone wrong”. There may be multiple potential causes. See the sample below for insights on how this may look in your PRA.
Step 4a- Using Table 2 above, use your cross-functional team to assign a quantitative value to the likelihood of this event occurring.
Step 4b- Using the Table 2 above, use your cross-functional team to assign a value for the severity of the consequence if this event were to occur.
Step 4c- Simply multiply your Likelihood and your Severity columns to create a Risk Score.
Step 5- Consider what possible additional controls could be effectively implemented to mitigate or control the risk.
Additional Notes:
Depending on your risk appetite, you may determine that the identified risk is acceptable in its current state, or you may choose to act on the risk. Hospitals will typically create their own scale for what level is acceptable and what level requires actions (Step 5).
Any Severity of 4 or 5 would usually require additional actions, with few exceptions. Many hospitals are shying away from creating a threshold, such as creating additional actions only for risk scores over 20. Historically, this lends to bias. The result is that many risks are scored less than 20 so as to avoid additional work.
Common rules of thumb for the PRA:
Determine your hospitals risk appetite based on the activity being analyzed.
Assemble the proper cross-functional team to assist in the PRA process.
Employ the usual ground rules for brainstorming in Step 1. If this step is wrong, everything else follows.
Assign as many potential impacts and potential causes as you see fit.
Determine your trigger for action, based on a high severity or a high Risk Score.
If you get stuck on a particular “thing gone wrong” analysis, maybe you need a different tool, such as the FMEA or Fishbone Diagram.
Show value in this process and find ways to link these activities of risk-based thinking to your cost of quality.
Summary:
Getting started with hospital risk-based thinking is easier than you think. You are already doing risk-based thinking, you just need easy access to meaningful tools to assist. The PRA is an entry-level tool for risk assessment. The PRA may be the only tool that you need for assessing risk at your hospital or you may need a more robust tool. Some hospitals will use the PRA as a screening tool to determine if a deeper dive for assessing risk is needed. The purpose of the PRA is to assist hospitals in managing risk. Managing hospital risk appropriately will help create a safer patient environment and allow all healthcare providers to keep their oath of “doing no harm”.